This material is intended for people without a medical education who want to know more about osteochondrosis than is written in popular publications and on the websites of private clinics. Patients ask questions to doctors of various specialties, which characterize a complete misunderstanding of the topic of osteochondrosis. Examples of such questions include: "why does osteochondrosis hurt me? "", "congenital osteochondrosis was discovered, what should I do? "Perhaps the apotheosis of such illiteracy can be considered a fairly common question: "Doctor, I have initial signs of chondrosis, how scary is it? "This article aims to structure the material about osteochondrosis, its causes, manifestations, methods of diagnosis, treatment and prevention, and to answer the most frequently asked questions. Since all of us, without exception, are patients with osteochondrosis, this article willbe useful to all.
What is osteochondrosis?
The name of the disease is scary when it is not clear. The medical suffix "-oz" means proliferation or enlargement of certain tissues: hyalinosis, fibrosis. An example would be cirrhosis of the liver, when the connective tissue increases and the functional tissue, the hepatocytes, decreases in volume. There may be an accumulation of pathological protein or amyloid that should not normally be present. This storage disease will be called amyloidosis. There may be significant enlargement of the liver due to fatty degeneration, which is called fatty hepatosis.
Well, it turns out that with intervertebral osteochondrosis, the cartilage tissue of the intervertebral discs increases in volume, because "chondros, χόνδρο" in translation from Greek to Russian means "cartilage"? No, chondrosis, or more precisely osteochondrosis, is not a disease of accumulation. In this case, there is no real growth of cartilage tissue, we are only talking about a change in the configuration of the intervertebral cartilage discs under the influence of many years of physical activity, and above we looked at what happens in each individual disc. The term "osteochondrosis" was introduced into the clinical literature by A. Hilderbrandt in 1933.
How do the biomechanics of a dehydrated disc change shape? As a result of excessive loading, their outer edges swell, tear and form protrusions, and then intervertebral hernias or cartilage nodes that go outside the normal contour of the disc. That is why chondrosis is called chondrosis, because cartilage nodes - hernias - occur where cartilage should not be, behind the outer contour of a healthy disc.
The edges of the vertebrae that are adjacent to the disc also hypertrophy, forming coracoids or osteophytes. Therefore, such a mutual violation of the configuration of cartilage and bone tissue is generally called osteochondrosis.
Osteochondrosis refers to dystrophic-degenerative processes and is part of the normal, normal aging of the intervertebral discs. None of us are surprised that the face of a 20-year-old girl will be slightly different from her face at the age of 70, but for some reason everyone believes that the spine, its intervertebral discs, are not subjected to the same pronouncedtemporary change. Dystrophy is a nutritional disorder, and degeneration is a disorder of the structure of the intervertebral discs after a long period of dystrophy.
Causes of osteochondrosis and its complications
The main cause of uncomplicated, physiological osteochondrosis can be considered the way a person moves: upright walking. Man is the only species on earth that walks on two legs among all mammals, and this is the only way of locomotion. Osteochondrosis became the scourge of humanity, but we freed our hands and created civilization. Thanks to upright walking (and osteochondrosis), we not only created the wheel, the alphabet and mastered fire, but you can also sit at home in the warmth and read this article on your computer screen.
Man's closest relatives, the higher primates - chimpanzees and gorillas, sometimes rise on two legs, but this mode of locomotion is auxiliary to them, and most often they still move on all fours. In order for osteochondrosis to disappear, similar to intensive aging of the intervertebral discs, a person must change his way of movement and remove the constant vertical load from the spine. Dolphins, killer whales and whales do not have osteochondrosis, and dogs, cows and tigers do not. Their spine does not take long-term static and shock vertical loads because it is in a horizontal position. If humanity goes to sea like Ichthyander and the natural mode of movement is diving, then osteochondrosis will be defeated.
The upright posture forced the human musculoskeletal system to evolve in the direction of protecting the skull and brain from shock loads. But the discs — the elastic pads between the vertebrae — aren't the only method of protection. A person has a springy arch of the foot, cartilage of the knee joints, physiological curves of the spine: two lordosis and two kyphosis. All this allows you not to "shake" your brain even while running.
Risk factors
But doctors are interested in those risk factors that can be modified and avoid the complications of osteochondrosis that cause pain, discomfort, limited mobility and reduced quality of life. Let's look at these risk factors that are so often overlooked by doctors, especially in private medical centers. After all, it is much more profitable to constantly treat a person than to indicate the cause of the problem, solve it and lose the patient. Here they are:
- the presence of longitudinal and transverse flat steps. Flat feet cause the arch of the foot to stop springing and the impact is transmitted up the spine without cushioning. Intervertebral discs experience significant stress and quickly collapse;
- overweight and obesity - no need to comment;
- improper lifting and carrying of heavy objects, with uneven pressure on the intervertebral discs. For example, if you lift and carry a bag of potatoes on one shoulder, then the intense load will fall on one edge of the discs and can be excessive;
- lack of physical activity and a sedentary lifestyle. It was said above that maximum pressure is exerted on the discs while sitting, since one never sits straight, but always "slightly" bends;
- chronic injuries, slipping on ice, intense weight lifting, contact martial arts, heavy hats, hitting your head on low ceilings, heavy clothing, carrying heavy bags.
Risk factors that can affect any person are listed above. Here we deliberately do not list diseases - connective tissue dysplasia, scoliotic deformity that changes the biomechanics of movement, Perthes disease and other conditions that aggravate and worsen the course of physiological osteochondrosis and lead to complications. These patients are treated by an orthopedist. What are the general symptoms of complicated osteochondrosis, for which patients turn to doctors?
General symptoms
The symptoms that will be described below exist outside of localization. These are common symptoms and can exist anywhere. These are pain, movement disorders and sensory disorders. There are also vegetative-trophic disorders or specific symptoms, for example, urination disorders, but much less often. Let's take a closer look at these signs.
Pain: muscular and radicular
Pain can be of two types: radicular and muscular. Radicular pain is associated with compression or squeezing of a protrusion or herniation of the intervertebral disc of the corresponding root at that level. Each nerve root consists of two parts: sensory and motor.
Depending on where exactly the hernia is directed and what part of the root is compressed, there may be sensory or motor disturbances. Sometimes both disorders appear at once, expressed to varying degrees. Pain also belongs to sensory disorders, because pain is a special, specific feeling.
Radicular pain: compression radiculopathy
Radicular pain is familiar to many; it is called "neuralgia". The swollen nerve root reacts violently to every stroke, and the pain is very sharp, similar to an electric shock. She shoots either the arm (from the neck) or the leg (from the lower back). Such a sharp, painful impulse is called lumbago: in the lower back it is lumbago, in the neck it is cervicago, a less common term. Such radicular pain requires forced, analgesic or antalgic posture. Radicular pain occurs immediately when coughing, sneezing, crying, laughing or straining. Any shock to the swollen nerve root causes an increase in pain.
Muscle pain: myofascial-tonic
But an intervertebral hernia or disc defect may not press on the nerve root, but when it moves, it can injure nearby ligaments, fascia, and deep muscles of the back. In this case, the pain will be secondary, painful, constant, stiffness will appear in the back, and such pain is called myofascial. The source of this pain will no longer be the nervous tissue, but the muscles. A muscle can only respond to any stimulus in one way: contraction. And if the stimulus is prolonged, the muscle contraction will turn into a constant spasm, which will be very painful.
A vicious circle is formed: the spasmodic muscle cannot be well supplied with blood, experiences oxygen starvation and poorly removes lactic acid, i. e. is. the product of its own vital activity, in the venous capillaries. And the accumulation of lactic acid again leads to an increase in pain. It is this type of muscular, chronic pain that significantly impairs the quality of life and forces the patient to undergo long-term treatment for osteochondrosis, although it does not prevent him from moving and does not force him to lie in bed.
A characteristic symptom of such secondary, myofascial pain will be increased stiffness in the neck, lower back or chest, the appearance of dense, painful muscle protrusions - "rollers" next to the spine, that is, paravertebral. In such patients, back pain intensifies afterseveral hours of "office" work, with prolonged immobility, when the muscles practically cannot work and are in a state of spasm.
Diagnosis of osteochondrosis
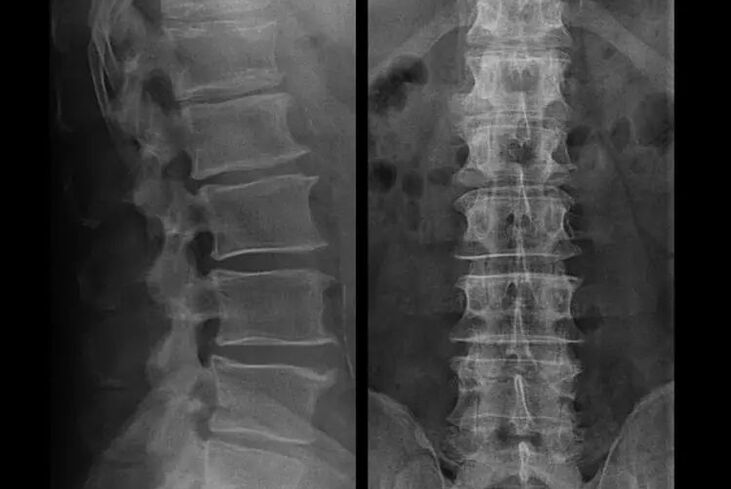
In typical cases, osteochondrosis of the cervical and cervical-thoracic spine manifests itself as described above. Therefore, the main stage of diagnosis was and remains the identification of the patient's complaints, establishing the presence of accompanying muscle spasm using a simple palpation of the muscles along the spine. Is it possible to confirm the diagnosis of osteochondrosis with an X-ray examination?
An "X-ray" of the cervical spine and even in functional tests of flexion and extension does not show cartilage, since their tissue transmits X-rays. However, based on the location of the vertebrae, general conclusions can be made about the height ofthe intervertebral discs, the general straightening of the physiological curvature of the neck - lordosis, as well as the presence of marginal growths of the vertebrae with prolonged irritation of theirfragile and dehydrated intervertebral disc surfaces Functional testing can confirm the diagnosis of cervical spine instability.
Since the discs themselves can only be seen with CT or MRI, magnetic resonance and X-ray computed tomography are indicated to clarify the internal structure of the cartilage and formations such as protrusions and hernias. Thus, with the help of these methods, an accurate diagnosis is made, and the result of the tomography is an indication and even an up-to-date guide for operative treatment of hernia in the neurosurgery department.
It should be added that no other research methods, apart from imaging, with the exception of MRI or CT, can show a hernia. Therefore, if you have been given a modern "computerized diagnosis" of the whole body, if the chiropractor has diagnosed you with a hernia by running his fingers along your back, if a hernia has been detected on the basis of acupuncture, a special extrasensory technique or a session of copper Thai massage, thenyou can immediately consider this level of diagnosis completely illiterate. Complications of osteochondrosis caused by bulging or hernia, compression, muscles, neurovascular, can only be treated by monitoring the condition of the intervertebral disc at an appropriate level.
Treatment of complications of osteochondrosis
Let's repeat once again that it is impossible to cure osteochondrosis, like planned aging and dehydration of the disc. You can simply not let things get complicated:
- if there are symptoms of narrowing of the height of the intervertebral discs, then you need to move properly, do not gain weight and avoid the appearance of protrusions and muscle pain;
- if you already have a protrusion, then you must be careful not to tear the fibrous ring, that is, not to transform the protrusion into a hernia and avoid the appearance of protrusions at several levels;
- if you have a hernia, then you should monitor it dynamically, take regular MRIs, avoid increasing the size or perform modern minimally invasive surgical treatment, since all conservative methods of treatment for exacerbation of osteochondrosis, without exception, leave the hernia in place andeliminating only temporary symptoms: inflammation, pain, shooting and muscle spasms.
But at the slightest violation of the regime, when lifting weights, hypothermia, injury, weight gain (in the case of the lower back), the symptoms return again and again. We will describe how you can deal with unpleasant sensations, pain and limited mobility in the back against the background of exacerbation of osteochondrosis and existing protrusion or hernia, due to socio-tonic syndrome.
What to do during a flare-up?
Since there was an attack of acute pain (for example, in the lower back), then you should follow the following instructions at the paramedical stage:
- complete elimination of physical activity;
- sleeping on a hard (orthopedic mattress or hard sofa), eliminating the sagging of the back;
- it is recommended to wear a semi-rigid corset to prevent sudden movements and "twists";
- On the lower back, you need to place a massage cushion with plastic needle applicators or use a Lyapko applicator. You need to hold it for 30 - 40 minutes, 2 -3 times a day;
- then NSAID-containing ointments, bee or snake venom ointments can be rubbed into the lower back;
- after rubbing, on the second day you can wrap the lower back with dry heat, for example, a dog hair belt.
A common mistake is to warm up on the first day. This can be a heating pad, bath procedures. At the same time, the swelling only increases, and along with it, the pain. You can warm up only after the "highest point of pain" has passed. Then the heat will enhance the "resorption" of the swelling. Usually this happens every 2-3 days.
The basis of any treatment is etiotropic therapy (eliminating the cause) and pathogenetic treatment (affecting the mechanisms of the disease). It is accompanied by symptomatic therapy. For vertebral pain (caused by problems in the spine), it goes like this:
- To reduce swelling of the muscles and spine, a salt-free diet and limiting the amount of fluid consumed is indicated. You can even give a mild potassium-sparing diuretic tablet;
- in the acute phase of lumbar osteochondrosis, short-term treatment can be carried out with intramuscular "injections" of NSAIDs and muscle relaxants: daily, 1. 5 ml intramuscularly for 3 days, 1 ml also intramuscularly for 5 days. This will help relieve the swelling of nerve tissue, eliminate inflammation and normalize muscle tone;
- in the subacute period, after overcoming the maximum pain, "injections" should no longer be taken and attention should be paid to restorative means, for example, modern drugs of group "B". They effectively restore impaired sensitivity, reduce stiffness and paresthesia.
Physiotherapy measures continue, it's time for exercise therapy for osteochondrosis. Its task is to normalize blood circulation and muscle tone when the swelling and inflammation have already disappeared, but the muscle spasm has not yet been completely resolved.
Kinesitherapy (treatment with movement) includes performing therapeutic gymnastics and swimming. Gymnastics for osteochondrosis of the cervical vertebrae is not aimed at the discs at all, but at the surrounding muscles. Its task is to relieve tonic spasm, improve blood flow and normalize venous outflow. This leads to a decrease in muscle tone, a decrease in the severity of pain and stiffness in the back.
Along with massage, swimming and acupuncture, it is recommended to purchase an orthopedic mattress and a special pillow. The pillow for osteochondrosis of the cervical spine should be made of a special material with "shape memory". Its task is to relax the muscles of the neck and suboccipital region, as well as to prevent blood flow disturbance at night in the vertebrobasilar region.
Autumn is an important stage in the prevention and treatment of home physiotherapy products and devices - from infrared and magnetic devices, to the most common needle applicators and ebonite discs, which are a source of weak electric currents during massage, which have a beneficial effect on a patient.
Exercises for osteochondrosis should be performed after a light general warm-up, on "warmed muscles". The main therapeutic factor is movement, not the degree of muscle contraction. Therefore, to avoid relapse, the use of a gymnastic mat and a gymnastic bar is not allowedWith their help, you can effectively restore range of motion.
Rubbing in ointments and using the Kuznetsov applicator continues. Swimming, underwater massage, Charcot shower are shown. During the fading stage of the exacerbation, home magnetic therapy drugs and physical therapy are indicated.
Usually, treatment takes no more than a week, but in some cases, osteochondrosis can manifest itself with such dangerous symptoms that surgery may be required urgently.
For Shantz's collar
In the early stages, during the acute stage, it is necessary to protect the neck from unnecessary movements. The Shants collar is great for this. Many people make two mistakes when buying this collar. They do not choose it according to its size, which is why it simply does not fulfill its function and causes a feeling of discomfort.

The second common mistake is long wearing for prophylactic purposes. This leads to weak neck muscles and only causes more problems. For a collar, there are only two indications in which it can be worn:
- the appearance of sharp pain in the neck, stiffness and pain spreading to the head;
- if you are going to do physical work in good health where there is a risk of "stretching" your neck and getting an aggravation. This is for example repairing a car when you lie down under it or washing windows when you have to reach out andtake awkward positions.
The collar should be worn for no more than 2-3 days, as longer wear may cause venous stasis in the neck muscles, at a time when it is time to activate the patient. An analogue of the Shants collar for the lower back is a semi-rigid corset purchased in an orthopedic salon.
Surgical treatment or conservative measures?
It is desirable that every patient, after the progression of symptoms, in the presence of complications, undergo an MRI and consult a neurosurgeon. Modern minimally invasive operations allow safe removal of fairly large hernias, without prolonged hospitalization, without being forced or lying down for several days, without disturbing the quality of life, because they are performed using modern video endoscopic, radio frequency, laser technology or withthe use of cold plasma. You can vaporize part of the core and reduce the pressure, reducing the risk of getting a hernia. And you can eliminate the defect radically, that is, by getting rid of it completely.
There is no need to be afraid to operate on hernias, these are no longer the previous types of open operations of the 80-90s of the last century with muscle dissection, blood loss and a subsequent long recovery period. They are rather a small puncture under X-ray control, followed by the use of modern technology.
If you prefer a conservative method of treatment, without surgery, then know that no method will allow you to reduce the hernia or remove it, no matter what they promise you! Neither hormonal injection, nor electrophoresis with papain, nor electrical stimulation, nor massage, nor the use of leeches, nor acupuncture can deal with a hernia. Creams and balms, kinesitherapy and even the introduction of platelet-rich plasma will not help either. And even traction therapy, or traction, for all its benefits, can only reduce symptoms.
That is why the motto for conservative treatment of intervertebral hernias can be the well-known expression "the minced meat can not return". The hernia can be eliminated only in time. The prices for modern operations are not so high, because they have to be paid once. But the annualtreatment in a sanatorium can ultimately cost 10-20 times more than the radical removal of a hernia with the disappearance of pain and restoration of the quality of life.
Prevention of osteochondrosis and its complications
Osteochondrosis, including the complex ones, the symptoms and treatment of which we considered above, for the most part is not a disease at all, but simply a manifestation of inevitable aging and premature "shrinking" of the intervertebral discs. Osteochondrosis needs little to avoid usconcerns:
- avoid hypothermia, especially in autumn and spring, and fall in winter;
- do not lift weights and carry loads only with a straight back, in a backpack;
- drink more clean water;
- do not gain weight, your weight should correspond to your height;
- treatment of flat feet, if any;
- do physical exercises regularly;
- performing types of exercises that reduce the load on the back (swimming);
- giving up bad habits;
- alternation of mental stress with physical activity. After every hour and a half of mental work, it is advisable to change the type of activity to physical work;
- You can regularly take at least an x-ray of the lumbar spine in two projections or an MRI to find out if the hernia is progressing, if any;
By following these simple recommendations, you can keep your back healthy and mobile for life.























